Diabetic Retinopathy
Diabetic Retinopathy is a condition occurring in persons with diabetes, which causes progressive damage to the retina, the light sensitive lining at the back of the eye. It is a serious sight-threatening complication of diabetes.
Diabetes is a disease that interferes with the body’s ability to use and store sugar, which can cause many health problems. Too much sugar in the blood can cause damage throughout the body, including the eyes. Over time, diabetes affects the circulatory system of the retina.
Diabetic retinopathy is the result of damage to the tiny blood vessels that nourish the retina. They leak blood and other fluids that cause swelling of retinal tissue and clouding of the vision. The condition usually affects both eyes. The longer a person has diabetes, the more likely they will develop diabetic retinopathy. If left untreated, diabetic retinopathy can cause blindness.

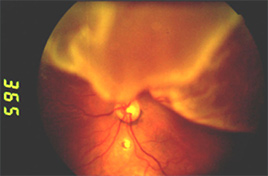
This is a healthy retina.

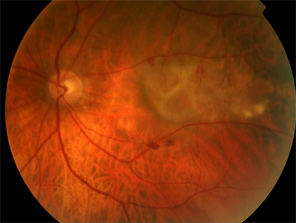
This is a retina of a patient with Diabetic Retinopathy.
Diabetic retinopathy can cause progressive, irreversible vision loss.
It is the leading cause of new cases of blindness in people.
Symptoms of diabetic retinopathy include:
- Seeing spots or floaters in your field of vision
- Blurred vision
- Having a dark or empty spot in the center of your vision
- Difficulty seeing well at night
In patients with diabetes, prolonged periods of high blood sugar can lead to the accumulation of fluid in the lens inside the eye that controls eye focusing. This changes the curvature of the lens and results in the development of symptoms of blurred vision. The blurring of distance vision as a result of lens swelling will subside once the blood sugar levels are brought under control. Better control of blood sugar levels in patients with diabetes also slows the onset and progression of diabetic retinopathy.
Often there are no visual symptoms in the early stages of diabetic retinopathy. This is why the American Optometric Association recommends that everyone with diabetes have a comprehensive dilated eye examination once a year. Early detection and treatment can limit the potential for significant vision loss from diabetic retinopathy.
Treatment of diabetic retinopathy varies depending on the extent of the disease. It may require laser surgery to seal leaking blood vessels or to discourage new leaky blood vessels from forming. Injections of medications into the eye may be needed to decrease inflammation or stop the formation of new blood vessels. It more advanced cases, a surgical procedure to remove and replace the gel-like fluid in the back of the eye, called the vitreous, may be needed. A retinal detachment, defined as a separation of the light-receiving lining in the back of the eye, resulting from diabetic retinopathy, may also require surgical repair.
If you are a diabetic, you can help prevent or slow the development of diabetic retinopathy by taking your prescribed medication, sticking to your diet, exercising regularly, controlling high blood pressure and avoiding alcohol and smoking.
What causes diabetic retinopathy?
Non-proliferative diabetic retinopathy (NPDR) is the early stage of the disease in which symptoms will be mild or non-existent. In NPDR, the blood vessels in the retina are weakened causing tiny bulges called microanuerysms to protrude from their walls.
Proliferative diabetic retinopathy (PDR) is the more advance form of the disease. At this stage, new fragile blood vessels can begin to grow in the retina and into the vitreous, the gel-like fluid that fills the back of the eye. The new blood vessel may leak blood into the vitreous, clouding vision.
Diabetic retinopathy is the result of damage caused by diabetes to the small blood vessels located in the retina. Blood vessels damaged from diabetic retinopathy can cause vision loss:
Fluid can leak into the macula, the area of the retina which is responsible for clear central vision. Although small, the macula is the part of the retina that allows us to see colors and fine detail. The fluid causes the macula to swell, resulting in blurred vision.
In an attempt to improve blood circulation in the retina, new blood vessels may form on its surface. These fragile, abnormal blood vessels can leak blood into the back of the eye and block vision.
Diabetic retinopathy is classified into two types:
- Non-proliferative diabetic retinopathy (NPDR) is the early stage of the blood disease in which symptoms will be mild or non-existent. In NPDR, the blood vessels in the retina are weakened causing tiny bulges called microanuerysms to protrude from their walls. The microanuerysms may leak fluid to the retina, which may lead to swelling of the macula.
- Proliferative diabetic retinopathy (PDR) is the more advanced form of the disease. At this stage, circulation problems cause the retina to become oxygen deprived. As a result new fragile blood vessels can begin to grow in the retina and into the vitreous, the gel-like fluid that fills the back of the eye. The new blood vessel may leak blood into the vitreous, clouding vision. Other complications of PDR include detachment of the retina due to scar tissue formation and the development of glaucoma. Glaucoma is a systemic disease defined as progressive damage to the optic nerve. In cases of proliferative diabetic retinopathy, the cause of this nerve damage is due to extremely high pressure in the eye. If left untreated, proliferative diabetic retinopathy can cause severe vision loss and even blindness.
Risk factors for diabetic retinopathy include:
- Diabetes – people with Type 1 or Type 2 diabetes are at risk for the development of diabetic retinopathy. The longer a person had diabetes, the more likely they are to develop diabetic retinopathy, particularly if the diabetes is poorly controlled.
- Race – Hispanic and African Americans are at greater risk for developing diabetic retinopathy.
- Medical Conditions – persons with other medical conditions such as high blood pressure and high cholesterol are at greater risk.
- Pregnancy – pregnant women face a higher risk for developing diabetes and diabetic retinopathy. If gestational diabetes develops, the patient is at much higher risk of developing diabetes as they age.
How is diabetic retinopathy diagnosed?
Diabetic retinopathy can be diagnosed through a comprehensive eye examination. Testing, with special emphasis on evaluation of the retina and macula, may include:
Patient history to determine vision difficulties experienced by the patient, presence of diabetes, and other general health concerns that may be affecting vision.
Visual acuity measurements to determine the extent to which central vision has been affected.
Refraction to determine the need for changes in an eyeglass prescription.
Evaluation of the ocular structures, including the evaluation of the retina through a dilated pupil.
Measurement of the pressure within the eye.
Supplemental testing may include:
Retinal photography or tomography to document current status of the retina.
Fluorescein angiography to evaluate abnormal blood vessel growth.
How is diabetic retinopathy treated?
Laser treatment (photocoagulation) is used to stop the leakage of blood and fluid in the retina. A laser beam of light can be used to create small burns in areas of the retina with abnormal blood vessels to try to seal the leaks.
Treatment for diabetic retinopathy depends on the stage of the disease and is directed at trying to slow or stop the progression of the disease.
In the early stages of Non-proliferative Diabetic Retinopathy, treatment other than regular monitoring may not be required. Following your doctor’s advice for diet and exercise and keeping blood sugar levels well-controlled can help control the progression of the disease.
If the disease advances, leakage of fluid from blood vessels can lead to macular edema. Laser treatment (photocoagulation) is used to stop the leakage of blood and fluid into the retina. A laser beam of light can be used to create small burns in the areas of the retina with abnormal blood vessels to try to seal the leaks.
When blood vessel growth is more widespread throughout the retina, as in proliferative diabetic retinopathy, a pattern of scattered laser burns is created across the retina. This causes abnormal blood vessels to shrink and disappear. With this procedure, some side vision may be lost in order to safeguard central vision.
Some bleeding into the vitreous gel may clear up on its own. However, if significant amounts of blood leak into the vitreous fluid in the eye, it will cloud vision and can prevent laser photocoagulation from being used. A surgical procedure called a vitrectomy may be used to remove the blood-filled vitreous and replace it with a clear fluid to maintain the normal shape and health of the eye.
Persons with diabetic retinopathy can suffer significant vision loss. Special low vision devices such as telescopic and microscopic lenses, hand and stand magnifiers, and video magnification systems can be prescribed to make the most of remaining vision.
Protecting Your Vision From Diabetes
The primary cause of legal blindness in the working population of the United States today is diabetes mellitus. Fourteen million Americans have this disease, 90% of whom have non-insulin dependent (Type II) diabetes, and 10% who have insulin-dependent (Type I) diabetes. Insulin-dependent diabetes typically occurs in people younger than 30, and requires regular insulin injections to live. Non-insulin dependent diabetes is most often observed in severely overweight adults and usually does not require insulin treatment.
Both types of diabetes can affect a person’s vision on many different levels, the most common complication being retinopathy. The earliest signs if diabetic retinopathy are observed when structural changes take place in the capillaries, thereby impending the flow of nutrients to the retina. The lack of nutrients and oxygen to the tissue result in damage to the retina. Many diabetics have few, if any, visual symptoms in the early stages of diabetic retinopathy, which is why it’s so critical to have regular, dilated eye exams every year.
Diabetes can also alter the clear tissue covering the front of the eye. Decreased corneal sensation has been noted and swelling of the corneal tissue can reduce vision, sometimes dramatically in people with this disease.
Overall, the risk of cataract is two to four times greater in diabetics as compared to those without the disease. In those with insulin-dependent (Type I) diabetes, the risk may be 15 to 25 times greater. Results of cataract surgery are quite good for patients who have no retinopathy; however, there seems to be a slightly higher risk of macular edema (swelling of the retinal tissue) after surgery in diabetics versus non-diabetics.
Temporary muscle paralysis of isolated muscles around the eye may occur is diabetes, and is frequently the initial clue to a latent diabetic condition. A person with this condition will often complain of “seeing double”, and as aggravating as that may be, a temporary solution (such as a patch) is sought since this condition usually resolves on its own in one to three months.
The first key in protecting your vision from the potential ravages of diabetes, is in close monitoring of your blood sugar. The Diabetes Control and Complications Trial (DCCT) determined that control of a patient’s blood sugar is critical in reducing the rate as well as progression of retinopathy. Diet and exercise are also essential components in maintaining tight control of your blood sugar. Your endocrinologist or internist should be able to help you design a regiment that works best for you.
The second element in safeguarding your vision is to get annual dilated eye exams with your eye doctor. As mentioned previously, early diabetic changes may not cause you any visual symptoms initially, but they still need to be closely monitored. Your optometrist is skilled in detecting any early diabetic changes in the eye, monitoring these changes, and referring you to a retinal specialist when necessary.
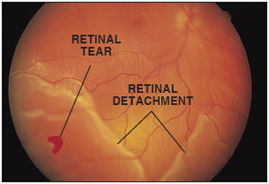
Retinal Detachment
Retinal Detachment is a separation of the retina (the inner nervous tunic of the eye) from the choroid (the middle, vascular tunic of the eye) in the back of the eye, usually resulting from a hole in the retina that allows the vitreous humor (fluid) to leak between the choroid and the retina.
Description of Retinal Detachment
The retina is a thin, transparent tissue of light-sensitive nerve fibers and cells. It covers the inside wall of the eye the same as wallpaper covers the walls of a room.
Most retinal detachments are caused by the presence of one or more small tears or holes in the retina. Normal aging can sometimes cause the retina to be thin and deteriorate, but more often shrinkage of the vitreous body, the clear gel-like substance which fills the center of the eye, is responsible for deterioration and retinal tears. The vitreous is firmly attached to the retina in several places around the back wall of the eye. As the vitreous shrinks, it may pull a piece of the retina away with it, leaving a tear or hole in the retina.
Though some shrinkage of the vitreous body occurs naturally with aging and usually causes no damage to the retina, abnormal growth of the eye (sometimes a result of nearsightedness), inflammation or injury, may also cause the vitreous to shrink. In most cases, a significant change in the structure of the vitreous body occurs before the development of a retinal detachment.
Once a retinal tear is present, watery fluid from the vitreous space may pass through the hole and flow between the retina and the back wall of the eye. This separates the retina from the back of the eye and causes it to “detach”. The part of the retina that is detached will not work properly and there will be a blind spot in vision.
Macular Degeneration
What is Macular Degeneration?
Age-related macular degeneration is the leading cause of blindness in the Unites States and many European countries. The neovascular “wet” form of the disease is responsible for most (90%) of the severe loss of vision.
There are approximately 200,000 new cases of wet macular degeneration in the United States each year. The average age of patients with the wet form of macular degeneration is the mid-70s. It rarely occurs before the age of 50. Wet macular degeneration is more common in whites, but occurs in all races.
 Picture of the fundus showing intermediate age-related macular degeneration
Picture of the fundus showing intermediate age-related macular degenerationWhat is age-related macular degeneration?
Age-related macular degeneration (AMD) is a disease associated with aging that gradually destroys sharp, central vision. Central vision is needed for seeing objects clearly and for common daily tasks such as reading and driving.
AMD affects the macula, the part of the eye that allows you to see fine detail. AMD causes no pain.
In some cases, AMD advances so slowly that people notice little change in their vision. In others, the disease progresses faster and may lead to a loss of vision in both eyes. AMD is a leading cause of vision loss in Americans 60 years of age and older.
AMD occurs in two forms: wet and dry.
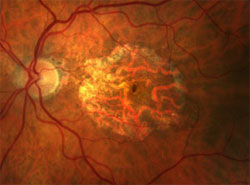
This is an advanced form of dry AMD in a small percentage of patients with “dry” AMD.
Fundus photograph of “wet” AMD
Where is the macula?
The macular is located in the center of the retina, the light-sensitive tissue at the back of the eye. The retina instantly converts light, or an image, into electrical impulses. The retina then sends these impulses, or nerve signals, to the brain.

What is wet AMD?
Wet AMD occurs when abnormal blood vessels behind the retina start to grow under the macula. These new blood vessels tend to be very fragile and often leak blood and fluid. The blood and fluid raise the macula from its normal place at the back of the eye. Damage to the macula occurs rapidly.
With wet AMD, loss of central vision can occur quickly. Wet AMD is also known as advanced AMD. It does not have stages like dry AMD.
An early symptom of wet AMD is that straight lines appear wavy. If you notice this condition or other changes to your vision, contact your eye care professional at once. You need a comprehensive dilated exam.
What is dry AMD?
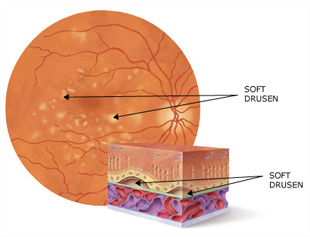
One key identifier for AMD is the collection of small, round, white-yellow, fatty deposits called drusen in the central part of the retina, the macula
Dry AMD occurs when the light-sensitive cells in the macula slowly break down, gradually blurring central vision in the affected eye. As dry AMD gets worse, you may see a blurred spot in the center of your vision. Over time, as less of the macula functions, central vision is gradually lost in the affected eye.
The most common symptom of dry AMD is slightly blurred vision. You may have difficulty recognizing faces. You may need more light for reading and other tasks. Dry AMD generally affects both eyes, but vision can be lost in one eye while the other eye seems unaffected.
One of the most common early signs of dry AMD is drusen.
What are Drusen?
Drusen are yellow deposits under the retina. They often are found in people over age 60. Your eye care professional can detect drusen during a comprehensive dilated eye exam.
Drusen alone do not usually cause vision loss. In fact, scientists are unclear about the connection between drusen and AMD. They do know that an increase in the size or number of drusen raises a person’s risk of developing either advances dry AMD or wet AMD. These changes can cause serious vision loss.
Dry AMD has three stages, all of which may occur in one or both eyes:
- Early AMD. People with early AMD have either several small drusen or a few medium-sized drusen. At this stage, there are no symptoms and no vision loss.
- Intermediate AMD. People with intermediate AMD have either many medium-sized drusen or one or more large drusen. Some people see a blurred spot in the center of their vision. More light may be needed for reading and other tasks.
- Advanced Dry AMD. In addition to drusen, people with advanced dry AMD have a breakdown of light-sensitive cells and supporting tissue in the central retinal area. This breakdown can cause a blurred spot in the center of your vision. Over time, the blurred spot may get bigger and darker, taking more of your central vision.
If you have vision loss from dry AMD in one eye only, you may not notice any changes in your overall vision. With the other eye seeing clearly, you still can drive, read, and see fine details. You may notice changes in your vision only if AMD affects both eyes. If blurriness occurs in your vision, see an eye care professional for a comprehensive dilated eye exam. Ninety percent of all people with AMD have this type. Scientists are still not sure what causes dry AMD.
What are the Symptoms of Macular Degeneration?
Diagnosing AMD
This is why Macular Degeneration is so dangerous, both dry and wet AMD cause NO pain.
For dry AMD: the most common early sign is blurred vision. As fewer cells in the macula are able to function, people will see details less clearly in front of them, such as faces or words in a book. Often this blurred vision will go away in brighter light. If the loss of these light-sensing cells becomes great, people may see a small-but growing- blind spot in the middle of their field of vision.
For wet AMD: the classic early symptom is that straight lines appear crooked. This results when fluid from the leaking blood vessels gathers and lifts the macula, distorting vision. A small blind spot may appear in wet AMD, resulting in loss of one’s central vision.
How is AMD detected?
Your eye care professional may suspect AMD if you are over age 60 and have had recent changes in your central vision. To look for signs of the disease, he or she will use eye drops to dilate, or enlarge your pupils. Dilating the pupils allows your eye care professional to view the back of the eye better.
AMD is detected during a comprehensive eye exam that includes:
- Visual acuity test. This eye chart test measures how well you see at various distances.
- Dilated eye exam. Drops are placed in your eyes to widen, or dilate, the pupils. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of AMD and other eye problems. After the exam, your close-up vision may remain blurred for several hours.
- Tonometry. An instrument measures the pressure inside the eye. Numbing drops may be applied to your eye for this test.
The doctors at Singer Haley Vision Center may do other tests to learn more about the structure and health of your eye.
During an eye exam, you may be asked to look at an Amsler grid. The pattern of the grid resembles a checkerboard. You will cover one eye and state at a black dot in the center of the grid. While staring at the dot, you may notice that the straight lines in the pattern appear wavy. You may notice that some of the lines are missing. These may be signs of AMD.
If the doctors at Singer Haley Vision Center think you need treatment for wet AMD, he or she may suggest a fluorescein angiogram. In this test, a special dye is injected into your arm. Pictures are taken as the dye passes through the blood vessels in your retina. The test allows your eye care professional to identify any leaking blood vessels and recommend treatment.
How is wet AMD treated?
Wet AMD can be treated with laser surgery, photodynamic therapy, and injections into the eye. None of these treatments is a cure for wet AMD. The disease and loss of vision may progress despite treatment.
- Laser surgery. This procedure uses a laser to destroy the fragile, leaky blood vessels. A high energy beam of light is aimed directly onto the new blood vessels and destroys them, preventing further loss of vision. However, laser treatment may also destroy some surrounding healthy tissue and some vision. Only a small percentage of people with wet AMD can be treated with laser surgery. Laser surgery is more effective if the leaky blood vessels have developed away from the fovea, the central part of the macula. Laser surgery is performed in a doctor’s office or eye clinic. The risk of new blood vessels developing after laser treatment is high. Repeated treatments may be necessary. In some cases, vision loss may progress despite repeated treatments.
- Photodynamic therapy. A drug called verteporfin in injected into your arm. It travels throughout the body, including the new blood vessels in your eye. The drug tends to “stick” to the surface of new blood vessels. Next, a light is shined into your eye for about 90 seconds. The light activates the drug. The activated drug destroys the new blood vessels and leads to slower rate of vision decline. Unlike laser surgery, this drug does not destroy surrounding healthy tissue. Because this drug is activated by light, you must avoid exposing your skin or eyes to direct sunlight or bright indoor light for five days after treatment. Photodynamic therapy is relatively painless. It takes about 20 minutes and can be performed in a doctor’s office. Photodynamic therapy slows the rate of vision loss. It does not stop vision loss or restore vision in eyes already damaged by advanced AMD. Treatment results often are temporary. You may need to be treated again.
- Injections. Wet AMD can now be treated with new drugs that are injected into the eye (anti-VEGF therapy). Abnormally high levels of a specific growth factor occur in eyes with wet AMD and promote the growth of abnormal new blood vessels. This drug treatment blocks the effects of the growth factor. You will need multiple injections that may be given as often as monthly. The eye is numbed before each injection. After the injection, you will remain in the doctor’s office for a while and you eye will be monitored. This drug treatment can help slow down vision loss from AMD and in some cases improve sight.
How is dry AMD treated?
Once dry AMD reaches the advanced stage, no form of treatment can prevent vision loss. However, treatment can delay and possibly prevent intermediate AMD from progressing to the advanced stage, in which vision loss occurs. The National Eye Institute’s Age-Related Eye Disease Study (AREDS) found that taking a specific high-dose formulation of antioxidants and zinc significantly reduces the risk of advanced AMD and its associated vision loss. Slowing AMD’s progression from the intermediate stage to the advanced stage will save the vision of many people.
Age-Related Eye Disease Study (AREDS)
What dosage of the AREDS formulation?
The specific daily amounts of antioxidants and zinc used by the study researchers were 500 milligrams of vitamin C, 400 International Units of vitamin E, 15 milligrams of beta-carotene (often labeled as equivalent to 25,000 International Units of vitamin A), 80 milligrams of zinc as zinc oxide, and two milligrams of copper as cupric oxide. Copper was added to the AREDS formulation containing zinc to prevent copper deficiency anemia, a condition associated with high levels of zinc intake.
Who should take the AREDS formulation?
People who are at high risk for developing advanced AMD should consider taking the formulation. You are at high risk for developing advanced AMD if you have either:
- Intermediate AMD in one or both eyes. OR
- Advanced AMD (dry or wet) in one eye but not in the other eye.
Your eye care professional can tell you if you have AMD, its stage, and your risk for developing the advanced form.
The AREDS formulation is not a cure for AMD. It will not restore vision already lost from the disease. However, it may delay the onset of advanced AMD. It may help people who are at high risk for developing advanced AMD keep their vision.
Can people with early stage AMD take the AREDS formulation to help prevent the disease from progressing to the intermediate stage?
There is no apparent need for those diagnosed with early stage AMD to take the AREDS formulation. The study did not find that the formulation provided a benefit to those with early stage AMD. If you have early stage AMD, a comprehensive dilated eye exam every year can help determine if the disease is progressing. If early stage AMD progresses to the intermediate stage, discuss taking the formulation with your doctor.
Can diet alone provide the same high levels of antioxidants and zinc as the AREDS formulation?
No. The high levels of vitamins and minerals are difficult to achieve from diet alone. However, previous studies have suggested that people who have diets rich in green leafy vegetables have a lower risk of developing AMD.
Can a daily multivitamin alone provide the same high levels of antioxidants and zinc as the AREDS formulation?
No. The formulation’s levels of antioxidants and zinc are considerably higher than the amounts in any daily multivitamin. If you are already taking daily multivitamins and your doctor suggests you take the high-dose AREDS formulations, be sure to review all your vitamin supplements with your doctor before you begin. Because multivitamins contain many important vitamins not found in the AREDS formulation, you may want to take a multivitamin along with the AREDS formulation. For example, people with osteoporosis need to be particularly concerned about taking vitamin D, which is not in the AREDS formulation.
How can I take care of my vision now that I have AMD?
Dry AMD
If you have dry AMD, you should have a comprehensive dilated eye exam at least once a year. Your eye care professional can monitor your condition and check for other eye diseases. Also, if you have intermediate AMD in one or both eyes, or advanced AMD in one eye only, your doctor may suggest that you take the AREDS formulation containing the high levels of antioxidants and zinc.
Because dry AMD can turn into wet AMD at any time, you should get an Amsler grid from your eye care professional. Use the grid every day to evaluate your vision for signs of wet AMD. This quick test works best for people who still have good central vision. Check each eye separately. Cover one eye and look at the grid. Then cover your other eye and look at the grid. If you detect any changes in the appearance of this grid or in your ever day vision while reading the newspaper or watching television, get a complete dilated eye exam.
Wet AMD
If you have wet AMD and your doctor advises treatment, do not wait. After laser surgery or photodynamic therapy, you will need frequent eye exams to detect any recurrence of leaking blood vessels. Studies show that people who smoke have a greater risk of recurrence than those who don’t. In addition, check your vision at home with the Amsler grid. If you detect any changes, schedule an eye exam immediately.
What can I do if I have already lost some vision from AMD?
If you have lost some sight from AMD, don’t be afraid to use your eyes for reading, watching TV, and other routine activities. Normal use of your eyes will not cause further damage to your vision. If you have lose some sight from AMD, ask your eye care professional about low vision services and devices that may help you make the most of your remaining vision. Ask for a referral to a specialist in low vision. Many community organizations and agencies offer information about low vision counseling, training, and other special services for people with visual impairments. A nearby school of medicine or optometry may provide low vision services.
Current Research
What research is being done?
The National Eye Institute is conducting and supporting a number of studies to learn more about AMD. For example, scientists are:
- Studying the possibility of transplanting healthy cells into a diseased retina.
- Evaluating families with a history of AMD to understand genetic and hereditary factors that may cause disease.
- Looking at certain anti-inflammatory treatments for the wet form of AMD.
This research should provide better ways to detect, treat, and prevent vision loss in people with AMD.
Singer Haley Vision: Louisiana LASIK & Cataract Surgery Leaders
FREE CONSULTATION
Services We Offer
- LASIK Surgery
- PRK Surgery
- CATARACT SURGERY
- PRK Surgery
- Glaucoma Surgery and Treatment
- Retina Surgery and Treatment



